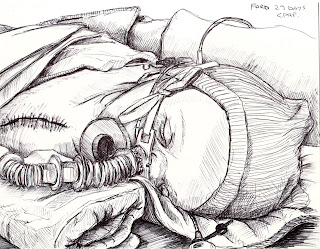
Ford is back in the ICU.
Having noticed his breathing becoming more difficult over the last two days, accompanied by a marked increase in his (by now habitual but still unnerving) retching and vomiting, a sudden jump in his weight (which is a sign of fluid build-up), and lower than usual oxygen
saturations, Christa decided to call the cardiology clinic and find out how worried we should be.
We were asked to come in and see the doctor and told to pack for a few days on the ward - just in case. But after a brief consult with Dr. Human, who confirmed our suspicions that Ford was indeed looking pretty bad, it was decided that the ICU would be a better choice for two reasons. The first being that they can keep a closer eye on him there than on the ward. If his condition takes a turn for the worse overnight they'll be in a better position to help him. The immediate plan for his treatment is to up his dosage of
diuretics to see if he'll pee off some of the excess fluid, get him on some minimal oxygen support to help his breathing, test for viruses that might be making him sick (he's already had his seasonal flu, H1N1, and RSV shots), and then sit tight and see if he improves. The second reason is that apparently during Cardiology's last big, collective meeting they brought up (
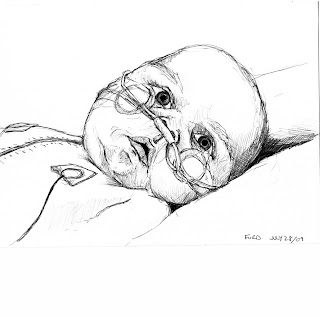
unbeknownst to us) the problem of Ford and what could/should be done to help him. It turns out they are not quite as thrilled with his progress as we are (we tried to impress on him how amazing Ford's smiling is, but he wasn't having any of it) and that his failure to thrive over the last 6 months complicates their long-term expectations.
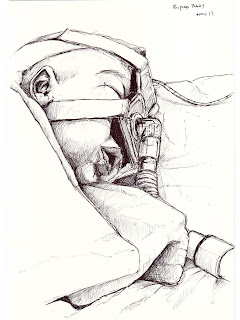
So now there is another surgery.
They are planning to put another shunt into Ford's heart, connecting his reconstructed aorta to the left side of his pulmonary artery. This will, in theory, bring an overall increase in blood flow to his lungs, raising his oxygen
saturations up to where they expected to see them post-Glenn, and also balance the blood that is being delivered to his lungs, bringing more to his left side, which has suffered from chronic collapse since his diaphragm surgeries and is also currently being neglected by the 'right-wing' anatomy of his "Glenn circulation."
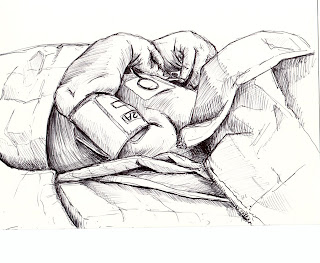
We are, as always, fuzzy on certain details, but it sounds as though they can do this procedure without cutting his chest open again, similar to how they did his diaphragm
plications, and we are relieved that he won't have to go through another open-heart surgery in the near future. It was impressed on us that they had no reason to wait to do this, that the last 6 months have shown them that Ford is committed to foiling their plans to fix him. So they might as well exhaust their options now and see if that finally gives him the impression that we are doing everything we can to keep him amongst the living, so he might as well stop resisting and join us. We're expecting this will happen as soon as next week and that Ford will remain in the ICU until then so that they can continue to efficiently manage him.
Christa and I had a little chat about whether or not we ought to bring up this next part of the story. I guess for us the word is clouded with fear and reverence, and given the many auspicious occasions we realized in hindsight that a little wood-knocking would have gone a long way, we are expectantly hesitant to throw it around. But in the end my penchant for drama and flair for epic blogging has won out, regardless of how much it angers the respective pantheons and phantasmagorias...
Dr.
Sanatani, another cardiologist who has been following Ford, was a little grim in his opinions this afternoon, suggesting that there were only two things left that they could do for Ford. If this shunt doesn't do the trick then we ought to list for a transplant.
Those of you who've been with us from the start might remember that we initially were given the choice to choose transplant as a primary treatment, instead of the 3-stage reconstruction, and that we had in fact chosen to go that route. It was subsequently impressed on us that transplants are a last-ditch effort, only to be used when you've exhausted other options, because you only get one shot at a transplant and they're a risky business at best. It's hard to believe that we could be coming full circle, that our initial logic for choosing a transplant over the surgeries he's been through was that it seemed much simpler. Just one surgery instead of 3. A whole heart instead of half, etc... and now after everything that's happened to Ford I feel like it's come back to haunt us and is sort of laughing from the shadows with an "I told you so" smirk. It's fair to point out that we aren't at that point yet, and that we knew it could come down to this, but to have it suddenly appear on the radar is terrifying.
I don't know if I can clearly express these complicated feelings that I have towards Ford, it's not that they are simply bittersweet. I have been feeling lately like I can't take much more of this, that ironically I am not made of the same stuff as him - maybe he's got more of his mom in him than me (I would hope so). I don't understand how a little body can take on so much and keep going. People say that he's a fighter but I've never been able to see it like that. All I see is this little being that is being beaten up, and that it lacks the capacity to see that it's not supposed to be like this, that most of us get off easy by comparison. To me that's more like being a lightning rod than a fighter. It's not a reciprocating force. It's just this little stick that can't help but be pummelled by an extremely damaging energy while the rest of us stand on the sidelines, oohing and awing. And then what am I supposed to do? I'm supposed to love this thing and hold it and nurture it. It's like grabbing onto a live power line and being unable to let go.