Saturday, November 28, 2009
5th times a charm?
Ford's 5th time under the knife went well, even though there were a few surprises.
First off, the bronchoscopy revealed no blockages in the lower airways of his left lung. So the promise of simply sucking out some kind of 'plug' to free up the lung was a bust.
However Dr. Campbell did notice, to his surprise, that Ford's left lung was completely encased in old, sticky chyle, which must have failed to drain back in September when they first noticed he might be suffering from a chylothorax (a cut lymph duct that leaks fatty fluid into the chest cavity). It was this stuff that had compromised the ability of his lung to fully expand and, I gather, in the intervening months slowly force it to quit altogether. He was surprised because this is something that they would have expected to see on an x-ray or a CT-scan, yet it had somehow gone unnoticed.
So he removed as much of it as he could, but got nervous as he closed in on the lung. He had to leave some of it around Ford's lower left lobe for fear of damaging healthy tissue.
The next issue was removing the collateral veins which had grown into the lung, competing with the antegrade flow from Ford's left pulmonary artery. There were many, as they suspected, and they were all cauterized without a hitch. Dr. Campbell then tried to impress us with the 'spectacular quality' of Ford's pulmonary artery, which I guess they suspected would be in rough shape, and we were impressed.
Next up he put in the 'BT Shunt' to supply more direct blood flow from the heart to the left pulmonary artery (which was supposed to be receiving passive flow via the 'Glenn' but was being entirely neglected in favour of the right lung).
Apparently that seemed to do the trick and Ford's oxygen saturations acutely jumped from 70% to 90%. Dr. Campbell explained that even though this is what they needed to have happen, they were hoping to trigger it without putting in the shunt (sucking out goo or freeing up space around the lung). This new modification will put an increased load on Ford's single ventricle, which is a bad thing in the long-run. They are worried that his heart has already been working harder than expected and that there might be some issues with it's function that will be exacerbated by the shunt. It's a wait and see sort of thing, from what i gather. Something they can assist with drugs but might end up becoming a big problem down the line (re: all this transplant talk of late).
Even though Ford performed well in the OR he's had a rough go since coming back to the ICU. His saturations slowly dropped back the 70's. The oxygen they're supplying him to compensate kept getting bumped up. He is very swollen and grey. They had just started him on a transfusion when we left, and everyone seemed convinced that it would do the trick.
The plan is to leave him intubated "for a while" keeping the pressure support high so that they can keep the lung open until it gets its strength back.
Friday, November 27, 2009
No surgery today
The surgery was postponed. Ford is second on the list for tomorrow, so it should happen sometime in the afternoon. He remains stable - sedated and intubated.
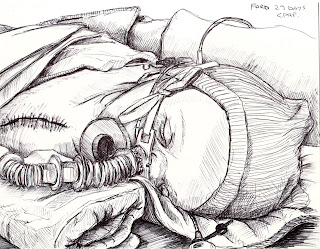
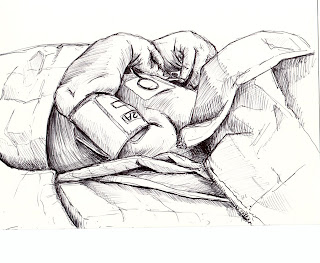
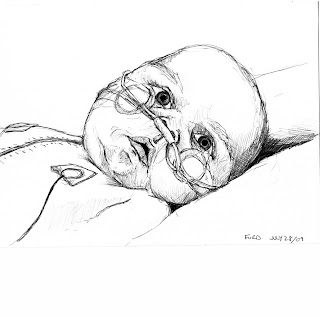
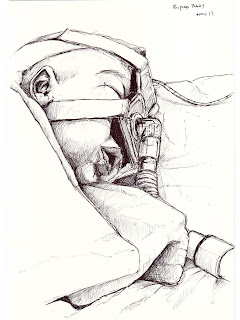
Meanwhile, in what is more an attempt to boost troop morale by prompting a flood of supportive and encouraging comments than a vanity project, please enjoy a selection of drawings I've made of Ford over the last few months (unfortunately he is easiest to draw while sedated, so they are bit biased in that regard).
Meanwhile, in what is more an attempt to boost troop morale by prompting a flood of supportive and encouraging comments than a vanity project, please enjoy a selection of drawings I've made of Ford over the last few months (unfortunately he is easiest to draw while sedated, so they are bit biased in that regard).




Thursday, November 26, 2009
halfsies
yesterday they put a picc line in Ford's arm - he's all out of veins for an iv start. since they'd be anaesthetizing him for that, they decided to do a cardiac cath to check his venous pressure while there.
they learned that the Glenn pressure is totally normal, but it's flow is entirely preferential to the right lung. they learned that, while they knew the blood flow to the left lung was bad (and he's got that pesky chronic left lower lobe collapse), that it is in fact "horrible". effectively, of late, he has been breathing with just his right lung.
"i think we all agree Ford is not well" said Dr. Sanatani last night, and indeed, one can hardly be expected to be well breathing with one lung and half a heart. yikes.
we basically had him at home, ie off any breathing support, long enough to totally tucker him out, and once we saw signs of respiratory distress, and were admitted back to the hospital, he's getting a chance to get some rest again, on the ventilator.
i hate seeing him intubated - they have to keep him sedated for it - but his colour is much better today because of it, and the mottling in his arms, which was severe yesterday, has also shown a marked improvement.
it is because the Glenn is only sending blood to the right lung that they are thinking of putting a shunt to the left pulmonary artery.
the thing is, if the lung is collapsed it can't ventilate blood anyway, regardless of what you send it.
also, part of doing Ford's Glenn so early on, was so that he no longer had the Sano shunt that they put in during his Norwood (first surgery). having a shunt increased the volume load of blood on the heart, and the thinking in the summer was that it was this increased workload that was keeping Ford from thriving.
so what's worse? no flow to the left lung? no, that's bad. or increased volume to the heart? hm, that's not great either.
which is why Sanatani dropped to "T word" on us - if there's no fix for this, Ford would need a transplant.
but they're going to try the shunt.
luckily to put the shunt in, they don't have to open his chest - they can go in from Ford's left side/back. he already has a scar there from the diaphragm plication - this will be a parallel incision slightly higher. also, he won't have to go on bypass for the procedure so that's good too. overall it's a less invasive procedure that his previous heart surgeries (you know you've seen the worse when sticking a shunt in your baby's heart doesn't seem like such a big deal).
while there, they are going to ventilate the left lung, and possibly perform a bronchoscopy to suction out any stuck goo, to try and open that lung fully so that it can do something with the blood that will be shunting to it. they're also going to remove all the collaterals that have formed, or as many that are accessible, to get rid of the conflicting blood flow - Ford's body, in an attempt to get blood to his lungs on its own, has grown a bunch of collateral veins. but we need the blood to forge on through the pulmonary artery. removing the collaterals will increase the flow in the PA.
performing this procedure won't make anything worse, but they aren't certain it will make anything better. it might, but there are so many variables in Ford that there is no clear path to proceed on. today plans kept changing as different doctors weighed in with their opinions, and it seems they are actually still somewhat in debate. when Dr. Campbell was describing the above plan, his train of thought kept wandering off into other possibilities and it was a bit of a confusing conversation as he included me in his thinking it through. later on, Dr. Human assured me they will come to a clear consensus before operating...
and they may operate tomorrow (friday) late afternoon, or on the weekend, TBD.
sooner is better than later in my opinion - Ford is just biding his time on the ventilator, and we're biding ours at his side, waiting for the next step.
they learned that the Glenn pressure is totally normal, but it's flow is entirely preferential to the right lung. they learned that, while they knew the blood flow to the left lung was bad (and he's got that pesky chronic left lower lobe collapse), that it is in fact "horrible". effectively, of late, he has been breathing with just his right lung.
"i think we all agree Ford is not well" said Dr. Sanatani last night, and indeed, one can hardly be expected to be well breathing with one lung and half a heart. yikes.
we basically had him at home, ie off any breathing support, long enough to totally tucker him out, and once we saw signs of respiratory distress, and were admitted back to the hospital, he's getting a chance to get some rest again, on the ventilator.
i hate seeing him intubated - they have to keep him sedated for it - but his colour is much better today because of it, and the mottling in his arms, which was severe yesterday, has also shown a marked improvement.
it is because the Glenn is only sending blood to the right lung that they are thinking of putting a shunt to the left pulmonary artery.
the thing is, if the lung is collapsed it can't ventilate blood anyway, regardless of what you send it.
also, part of doing Ford's Glenn so early on, was so that he no longer had the Sano shunt that they put in during his Norwood (first surgery). having a shunt increased the volume load of blood on the heart, and the thinking in the summer was that it was this increased workload that was keeping Ford from thriving.
so what's worse? no flow to the left lung? no, that's bad. or increased volume to the heart? hm, that's not great either.
which is why Sanatani dropped to "T word" on us - if there's no fix for this, Ford would need a transplant.
but they're going to try the shunt.
luckily to put the shunt in, they don't have to open his chest - they can go in from Ford's left side/back. he already has a scar there from the diaphragm plication - this will be a parallel incision slightly higher. also, he won't have to go on bypass for the procedure so that's good too. overall it's a less invasive procedure that his previous heart surgeries (you know you've seen the worse when sticking a shunt in your baby's heart doesn't seem like such a big deal).
while there, they are going to ventilate the left lung, and possibly perform a bronchoscopy to suction out any stuck goo, to try and open that lung fully so that it can do something with the blood that will be shunting to it. they're also going to remove all the collaterals that have formed, or as many that are accessible, to get rid of the conflicting blood flow - Ford's body, in an attempt to get blood to his lungs on its own, has grown a bunch of collateral veins. but we need the blood to forge on through the pulmonary artery. removing the collaterals will increase the flow in the PA.
performing this procedure won't make anything worse, but they aren't certain it will make anything better. it might, but there are so many variables in Ford that there is no clear path to proceed on. today plans kept changing as different doctors weighed in with their opinions, and it seems they are actually still somewhat in debate. when Dr. Campbell was describing the above plan, his train of thought kept wandering off into other possibilities and it was a bit of a confusing conversation as he included me in his thinking it through. later on, Dr. Human assured me they will come to a clear consensus before operating...
and they may operate tomorrow (friday) late afternoon, or on the weekend, TBD.
sooner is better than later in my opinion - Ford is just biding his time on the ventilator, and we're biding ours at his side, waiting for the next step.
Tuesday, November 24, 2009
There and back again

Ford is back in the ICU.
Having noticed his breathing becoming more difficult over the last two days, accompanied by a marked increase in his (by now habitual but still unnerving) retching and vomiting, a sudden jump in his weight (which is a sign of fluid build-up), and lower than usual oxygen saturations, Christa decided to call the cardiology clinic and find out how worried we should be.
We were asked to come in and see the doctor and told to pack for a few days on the ward - just in case. But after a brief consult with Dr. Human, who confirmed our suspicions that Ford was indeed looking pretty bad, it was decided that the ICU would be a better choice for two reasons. The first being that they can keep a closer eye on him there than on the ward. If his condition takes a turn for the worse overnight they'll be in a better position to help him. The immediate plan for his treatment is to up his dosage of diuretics to see if he'll pee off some of the excess fluid, get him on some minimal oxygen support to help his breathing, test for viruses that might be making him sick (he's already had his seasonal flu, H1N1, and RSV shots), and then sit tight and see if he improves. The second reason is that apparently during Cardiology's last big, collective meeting they brought up (unbeknownst to us) the problem of Ford and what could/should be done to help him. It turns out they are not quite as thrilled with his progress as we are (we tried to impress on him how amazing Ford's smiling is, but he wasn't having any of it) and that his failure to thrive over the last 6 months complicates their long-term expectations.
So now there is another surgery.
They are planning to put another shunt into Ford's heart, connecting his reconstructed aorta to the left side of his pulmonary artery. This will, in theory, bring an overall increase in blood flow to his lungs, raising his oxygen saturations up to where they expected to see them post-Glenn, and also balance the blood that is being delivered to his lungs, bringing more to his left side, which has suffered from chronic collapse since his diaphragm surgeries and is also currently being neglected by the 'right-wing' anatomy of his "Glenn circulation."
We are, as always, fuzzy on certain details, but it sounds as though they can do this procedure without cutting his chest open again, similar to how they did his diaphragm plications, and we are relieved that he won't have to go through another open-heart surgery in the near future. It was impressed on us that they had no reason to wait to do this, that the last 6 months have shown them that Ford is committed to foiling their plans to fix him. So they might as well exhaust their options now and see if that finally gives him the impression that we are doing everything we can to keep him amongst the living, so he might as well stop resisting and join us. We're expecting this will happen as soon as next week and that Ford will remain in the ICU until then so that they can continue to efficiently manage him.
Christa and I had a little chat about whether or not we ought to bring up this next part of the story. I guess for us the word is clouded with fear and reverence, and given the many auspicious occasions we realized in hindsight that a little wood-knocking would have gone a long way, we are expectantly hesitant to throw it around. But in the end my penchant for drama and flair for epic blogging has won out, regardless of how much it angers the respective pantheons and phantasmagorias...
Dr. Sanatani, another cardiologist who has been following Ford, was a little grim in his opinions this afternoon, suggesting that there were only two things left that they could do for Ford. If this shunt doesn't do the trick then we ought to list for a transplant.
Those of you who've been with us from the start might remember that we initially were given the choice to choose transplant as a primary treatment, instead of the 3-stage reconstruction, and that we had in fact chosen to go that route. It was subsequently impressed on us that transplants are a last-ditch effort, only to be used when you've exhausted other options, because you only get one shot at a transplant and they're a risky business at best. It's hard to believe that we could be coming full circle, that our initial logic for choosing a transplant over the surgeries he's been through was that it seemed much simpler. Just one surgery instead of 3. A whole heart instead of half, etc... and now after everything that's happened to Ford I feel like it's come back to haunt us and is sort of laughing from the shadows with an "I told you so" smirk. It's fair to point out that we aren't at that point yet, and that we knew it could come down to this, but to have it suddenly appear on the radar is terrifying.
I don't know if I can clearly express these complicated feelings that I have towards Ford, it's not that they are simply bittersweet. I have been feeling lately like I can't take much more of this, that ironically I am not made of the same stuff as him - maybe he's got more of his mom in him than me (I would hope so). I don't understand how a little body can take on so much and keep going. People say that he's a fighter but I've never been able to see it like that. All I see is this little being that is being beaten up, and that it lacks the capacity to see that it's not supposed to be like this, that most of us get off easy by comparison. To me that's more like being a lightning rod than a fighter. It's not a reciprocating force. It's just this little stick that can't help but be pummelled by an extremely damaging energy while the rest of us stand on the sidelines, oohing and awing. And then what am I supposed to do? I'm supposed to love this thing and hold it and nurture it. It's like grabbing onto a live power line and being unable to let go.
Thursday, November 19, 2009
Home again, home again. Jiggity jig.
So my plan to set everyone straight seems to have worked, regardless of how reckless it may turn out to be (ie: dinner table). We were discharged Wednesday afternoon and have slowly been readjusting to Ford's presence at home. My initial, impulsive impressions were correct: We could not tolerate another rotation of the "Blue Team" pediatricians, comprised mostly of student interns and junior residents, who seem more interested in impressing their superiors than in taking care of Ford. The morning rounds were, at times, almost embarrassing, with us having to repeatedly impose ourselves onto the conversation to preserve some semblance of accuracy towards his condition: No, he is not 7 months old; no, he is not tolerating is oral feeds "really well," he doesn't take food orally; no, he hasn't regained full use of his right arm, he hardly uses it; no, he isn't taking 50mg of Blahblahblahbitol, please don't up his dose of that, you've got your patients mixed up, etc. Not that I'm tooting my own horn, here. It's just that this last stay in the hospital has brought home the importance of the expression: You are your child's advocate. Which was at first a horribly overwhelming abstraction, and is now, I feel, the only thing standing between Ford and another 6 months on the ward.
Not that we are the competent professionals we blame the residents for not being. This evening, for example, we had to frantically page both the Cardiologist and Neurologist on-call because Ford's evening dose of Phenobarbitol got lost in the day's chaos, and the pharmacy where Christa dropped it off closed before we could get there. In a pinch, it appears, no 24 pharmacy in the city can make Phenobarbitol for you, despite a doctor's willingness to fax in a prescription. So we had to haggle with the ER's charge nurse to let us come and pick up a free dose prepared by the hospital, without ever actually confirming with them the presence of an actual patient (Ford was at home, comfortably sleeping - not on the dinner table):
(a snippet of the conversation in the ER)
Me: I'm here to pick up a dose of Phenobarbitol for my son. My wife called the Neurologist and they said you would make it for us.
Nurse 1: Umm. ok. Is this an emergency? Where is your son?
Me: He's not here. He's at home sleeping.
Nurse 1: Umm... Ok. I don't think I can help you...
Me: I was told to ask for "Jerry"
Nurse 1: ...Ok. Well, you can go ask for her at the Nursing station.
Me: Hi. I need to speak to Jerry about getting some Phenobarb (note my casual abbreviation)
Nurse 2: Oh. Ok. Here. We have a note saying: Mom to pick up Phenobarbitol for Ford.
Me: Yeah, that's it.
Nurse 2: Ok, I'll just cross out "mom" and put... umm.. "dad"?
Me: Sure. Great.
Nurse 2: Ok. Well I hope it's the right dose.
Me: Yeah, yeah. Thanks. Do I need to sign anything?
Nurse 2: Umm... nope. I'll just put "dad" down here.
Me: Ok, great. See ya.
Moonlighting as a drug-pusher in a children's hospital ER, before making a speeding exit in a taxi, is not what I had in mind when I thought I'd like to "have kids."
I guess we're still learning. I hope the progress is exponential, otherwise Ford is in for a doubly rough start.
_______________________________________
(A self-indulgent treat that I'd like to share with all the grandparents out there)
Though I believe Grandma Corinne gets full credit for coaxing the first smile out of Ford post-stroke, I credit the second one to dancing around the room with him to this song.
Nothing's warmed my heart more these last few days than watching his face light up as we spin around together. I was prepared to accept that he might never smile again, having had to endure this last ordeal. It hurt so much the first time I saw him crack a grin, it was like being punched in the face. I hope that gets all you old fogies smiling as much as it did the young baby (and perhaps all the rest of us in between, too).
Tuesday, November 17, 2009
beautiful!
Monday, November 16, 2009
Escape from the Ward
 We were moved back upstairs to the ward on Saturday afternoon and have since been stuck in an uncomfortable limbo. Neurology seems confident that Ford's seizures have been tamed by the Phenobarbitol, Hematology is happy with the dosage of Enoxaparin, Cardiology thinks Ford is doing as well as he ever has (despite his bouts of heart-block, which have probably been happening the whole time we were at home anyway, and for which they are basically planning to do nothing), Gastroenterology wants to see him in a month in their clinic, we have already been in touch with a community based OT/PT who can follow Ford from home, his feeds have been weaned back up their previous rate, his two weeks of oral antibiotics are almost done, he's got no infections, viruses, etc, AND SO... Why are we still here?
We were moved back upstairs to the ward on Saturday afternoon and have since been stuck in an uncomfortable limbo. Neurology seems confident that Ford's seizures have been tamed by the Phenobarbitol, Hematology is happy with the dosage of Enoxaparin, Cardiology thinks Ford is doing as well as he ever has (despite his bouts of heart-block, which have probably been happening the whole time we were at home anyway, and for which they are basically planning to do nothing), Gastroenterology wants to see him in a month in their clinic, we have already been in touch with a community based OT/PT who can follow Ford from home, his feeds have been weaned back up their previous rate, his two weeks of oral antibiotics are almost done, he's got no infections, viruses, etc, AND SO... Why are we still here?We seem to be at the mercy of the dreaded 'charge nurse' and the junior pediatric resident, and god know's why they're suddenly in charge. As we've repeatedly experienced, right from the get-go to this very day, whenever someone new assesses Ford they panic: Oh he's really blue, he's struggling to breath, he has an erratic heart rhythm, he's not feeding well, he's so far behind in his development, ergo: this kid is really sick! Well, no kidding. But we've got the dismissive farewell blessing from 1-2-3-4 teams of specialists, who all think that he's as well as he's going to be right now, he's not being actively treated for anything, by anyone, and in the meantime we are forced to suffer through the exhausting routine of hospital living. Two weeks ago, when Ford's surgeon cheerily suggested that we take the opportunity to check into the ward for 48 hours of antibiotics and some respite I wanted to smack him. RESPITE? I'm not sure what he does for relaxation, but confining yourself to a prison-cell-sized room, voluntarily giving up all your privacy, tying your kid to his bed, forcibly restraining said kid so they can frequently stab, squeeze, prod, pinch, and irritate him, subjecting yourself to torturous nights of hourly wake-up calls on top of a fussing baby, amounts to something more like hell than a vacation in the Bahamas...
There is currently a dour clump of doctors slinking through the halls, slowly making their way to our room for Monday morning rounds. I'm really hoping I can talk some sense into them (or if nothing else impress upon them how unnecessary and agonizing this is for the 3 of us), and reclaim some control from the anxious, green med students, and policy-Nazis who've hijacked control of this ward. We just want to go home.
To end on a happier note, we've been afforded some real, high-quality respite care from the recent arrival of Grandma Corrine, who's taken to sitting with Ford in the afternoons so we can make some of the many and much needed changes to our home - to better accommodate Ford. We're really thankful for her offering to make the long drive up from California, for her relentless optimism, and for her patience and understanding when faced with our frayed nerves and wit's-end behavior. We're actually thankful for the help that all of you have given us over the last 6 months, here or there or elsewhere, or just in reading the blog from time to time and keeping us committed to updating it.
Friday, November 13, 2009
progress
today was a good day.
Ford was switched from bi-pap to c-pap in a move towards weaning him off entirely. the thinking at rounds is that he could be off c-pap by monday. late morning, our nurse took off the mask to wash his face, and as he was SO very happy as soon as it came off, she gave him a good 15 minute break. during that time his sats and work of breathing remained stable.
Vik, the resident following Ford, is a bit of a douche, as Nick put it. we tend to ignore what he has to say and wait until one of the doctors who's thinking is more inline with our own comes by to press for changes we feel are right for Ford. he was the one with this whole wean-by-monday plan. he admitted he was being overly cautious, concerned about Ford's left lung lower lobe collapse. i explained Ford has chronic atelectasis but he blew that off, as he does most things we say, simply, it would seem, so he can resume talking, which he prefers to listening. luckily, he ran his plan by Mona, the fellow, who thought since he did so well off for 15 minutes, why not try 2 hours. yay!
Ford is a different baby off bi-pap - content and social. i think having the mask on must be depressing, and he tries his best just to hunker down and wait it out when it's on. this is what it looks like - so i can't blame him for being so unsettled with it:
it was wonderful to see so much of his face when it came off. i missed it these past few days.
though he was much more relaxed without the mask, he certainly doesn't seem like his "old self". kind of too relaxed - like out of it relaxed. we have to remind ourselves it is too soon to worry much about that though - it has only been 8 days since his stroke, and his body is still adjusting to the phenobarbital, which makes you a bit dopey. soon, that effect will subside and soon he will be well into healing from this most recent trauma.
near the end of his 2 hour break, he fell asleep on his tummy. happily, Mary, the intestivist, happened to be near by observing Ford's wenckebach (oh yeah - he now spontaneously goes into wenckebach no where near his dose of carvedilol) and she commented (and we made her write it down) that Ford did not have to go back on c-pap at all, as long as he remained comfortable. hurrah!
this bouyed my spirits greatly as, if he can swing 24 hours off c-pap, we can go upstairs and be that much closer to getting back home.
my mom arrived from California last night, so we left he with Ford in the evening and came home early for some much welcome decompressing time.
Ford was switched from bi-pap to c-pap in a move towards weaning him off entirely. the thinking at rounds is that he could be off c-pap by monday. late morning, our nurse took off the mask to wash his face, and as he was SO very happy as soon as it came off, she gave him a good 15 minute break. during that time his sats and work of breathing remained stable.
Vik, the resident following Ford, is a bit of a douche, as Nick put it. we tend to ignore what he has to say and wait until one of the doctors who's thinking is more inline with our own comes by to press for changes we feel are right for Ford. he was the one with this whole wean-by-monday plan. he admitted he was being overly cautious, concerned about Ford's left lung lower lobe collapse. i explained Ford has chronic atelectasis but he blew that off, as he does most things we say, simply, it would seem, so he can resume talking, which he prefers to listening. luckily, he ran his plan by Mona, the fellow, who thought since he did so well off for 15 minutes, why not try 2 hours. yay!
Ford is a different baby off bi-pap - content and social. i think having the mask on must be depressing, and he tries his best just to hunker down and wait it out when it's on. this is what it looks like - so i can't blame him for being so unsettled with it:
it was wonderful to see so much of his face when it came off. i missed it these past few days.
though he was much more relaxed without the mask, he certainly doesn't seem like his "old self". kind of too relaxed - like out of it relaxed. we have to remind ourselves it is too soon to worry much about that though - it has only been 8 days since his stroke, and his body is still adjusting to the phenobarbital, which makes you a bit dopey. soon, that effect will subside and soon he will be well into healing from this most recent trauma.
near the end of his 2 hour break, he fell asleep on his tummy. happily, Mary, the intestivist, happened to be near by observing Ford's wenckebach (oh yeah - he now spontaneously goes into wenckebach no where near his dose of carvedilol) and she commented (and we made her write it down) that Ford did not have to go back on c-pap at all, as long as he remained comfortable. hurrah!
this bouyed my spirits greatly as, if he can swing 24 hours off c-pap, we can go upstairs and be that much closer to getting back home.
my mom arrived from California last night, so we left he with Ford in the evening and came home early for some much welcome decompressing time.
Wednesday, November 11, 2009
Daily Maintanence
Minor updates...
Ford has been moving in and out of 'heart block' over the last few days. I believe they first noticed it after restarting his regular medications, which were held for a few days following his seizures. Cardiology is seemingly scratching their heads as to why this has happened. The irregular rhythms are timed with his doses of metroprolol, one of the heart drugs he's been on for months now and has never reacted badly to before. The unsatisfying shrugs, followed by: well, we know he did this after his Glen, so we're not really worried, were accompanied with a pro-active change in his medications today. But unfortunately the new drug, carvedilol, also seemed to trigger the same funky rhythm immediately after it was given this evening.
The weird rhythm, called "winky back" (causing Christa and I to snicker and mutter off-coloured jokes about the "science" of cardiology), is actually "Wenckebach" (causing Christa and I to feel embarrassed and sit quietly while we are schooled by the science of cardiology), which causes a strange phasing of the electrical signals in his heart across several beats, eventually getting so far out of sync that he drops a beat. Even though his heart rate quickly slows from the 140's to the 80's shortly after the heart block kicks in, as longs as he doesn't exhibit any other signs of distress (extreme drop in blood pressure, drop in O2 sats, cyanosis, etc) he isn't in any immediate danger of kicking the bucket (incidentally, kicking-the-bucket is another misappropriated term from the dictionary of cardiology, which actually refers to Willem Kikntëbôkt, a 16th C. Swedish anatomist who first theorized the link between Incomplete Kardiac Electrical Activity and imminent death. If you don't believe me, type 'IKEA' into wikipedia for a disambiguous reference)
Next up, I ought to have knocked-on-wood when I pandered to the now relatively insignificant status of Ford's lung function in my last post, for today, spurned and enraged, they decided to exhibit their wrath via a pleural effusion - which is a leaking of fluid into the pleural cavity that surrounds the lungs. This can be very dangerous if it is not immediately treated with the surgical insertion of a drainage tube into the chest, but since neurology is anxious that Ford not go through any more surgeries in the near future (though this mostly applies to heart surgeries), folks seem reluctant to go that route. And assuming the effusion remains minor it should be successfully removed by the increase in his diuretics that they ordered this morning and a longer than expected wean from the Bipap.
Behaviourally, Ford was much more alert today than he has been since the seizures. Even though the bipap mask obscures most of his head, forces him into an almost constant cross-eyed stare, blows cold, pressurized air all over his face, and prompts him to produce disgusting amounts of frothy, bubbling drool (or "happy bubbles" as well like to call them), he managed to remain awake and calm for an unusually long period of time. We spent much of the day reading to him (Christa from "Global Babies" and I from "Under the Volcano"), to try and stimulate and/or salvage his "speech and language" centre. As well as lots of cuddles and play time, paying particular attention to his right arm, which was moving more today than it yet has, but is still pretty much dead weight.
And so it goes.
Ford has been moving in and out of 'heart block' over the last few days. I believe they first noticed it after restarting his regular medications, which were held for a few days following his seizures. Cardiology is seemingly scratching their heads as to why this has happened. The irregular rhythms are timed with his doses of metroprolol, one of the heart drugs he's been on for months now and has never reacted badly to before. The unsatisfying shrugs, followed by: well, we know he did this after his Glen, so we're not really worried, were accompanied with a pro-active change in his medications today. But unfortunately the new drug, carvedilol, also seemed to trigger the same funky rhythm immediately after it was given this evening.
The weird rhythm, called "winky back" (causing Christa and I to snicker and mutter off-coloured jokes about the "science" of cardiology), is actually "Wenckebach" (causing Christa and I to feel embarrassed and sit quietly while we are schooled by the science of cardiology), which causes a strange phasing of the electrical signals in his heart across several beats, eventually getting so far out of sync that he drops a beat. Even though his heart rate quickly slows from the 140's to the 80's shortly after the heart block kicks in, as longs as he doesn't exhibit any other signs of distress (extreme drop in blood pressure, drop in O2 sats, cyanosis, etc) he isn't in any immediate danger of kicking the bucket (incidentally, kicking-the-bucket is another misappropriated term from the dictionary of cardiology, which actually refers to Willem Kikntëbôkt, a 16th C. Swedish anatomist who first theorized the link between Incomplete Kardiac Electrical Activity and imminent death. If you don't believe me, type 'IKEA' into wikipedia for a disambiguous reference)
Next up, I ought to have knocked-on-wood when I pandered to the now relatively insignificant status of Ford's lung function in my last post, for today, spurned and enraged, they decided to exhibit their wrath via a pleural effusion - which is a leaking of fluid into the pleural cavity that surrounds the lungs. This can be very dangerous if it is not immediately treated with the surgical insertion of a drainage tube into the chest, but since neurology is anxious that Ford not go through any more surgeries in the near future (though this mostly applies to heart surgeries), folks seem reluctant to go that route. And assuming the effusion remains minor it should be successfully removed by the increase in his diuretics that they ordered this morning and a longer than expected wean from the Bipap.
Behaviourally, Ford was much more alert today than he has been since the seizures. Even though the bipap mask obscures most of his head, forces him into an almost constant cross-eyed stare, blows cold, pressurized air all over his face, and prompts him to produce disgusting amounts of frothy, bubbling drool (or "happy bubbles" as well like to call them), he managed to remain awake and calm for an unusually long period of time. We spent much of the day reading to him (Christa from "Global Babies" and I from "Under the Volcano"), to try and stimulate and/or salvage his "speech and language" centre. As well as lots of cuddles and play time, paying particular attention to his right arm, which was moving more today than it yet has, but is still pretty much dead weight.
And so it goes.
Tuesday, November 10, 2009
mon petit chou
Finally got to meet with a Neurologist.
She confirmed the relative good news that while nothing had gotten any better, things hadn't gotten worse.
The treatment for his venous sinus thrombosis (brain vein clots), was downgraded from Heparin to Enoxaparin, which is easier on his system long-term, and poses a lower risk of starting new bleeds. The existing clots will take months to break down, if they do at all. She said that only 60-70% tend to fully dissolve and that if they don't the blood will form/find new ways to get out of his head. This happened with Ford's first clot (in his left femoral vein, back in Edmonton), where the blockage has remained but his body has grown multiple collateral connections around it to keep the blood supply moving. This has also happened throughout his chest, prompted by lower than normal oxygen saturation, where (according to his surgeon) a surprising number of collateral pathways had grown into his lungs with the hopes of boosting their blood supply. So from this point of view, Neurology is only interested in seeing Ford in about 3 months time (assuming the seizures don't come back) to do a repeat CT scan and see if there has been any progress in breaking things down.
We were, of course, mostly concerned with how damaging this has been for him and how much loss of function we should expect. Unfortunately it's pretty grey and she was reluctant to give us any definitive answers. But, similar to his circulatory system, if parts of the brain get damaged new pathways are developed. She emphasized the plasticity of infant brains, suggesting that his brain will likely prioritize its functions and make sure that things which are high-priority (like speech and language) get moved to less damaged areas, but that this comes at the price of loosing other abilities that would otherwise occupy those regions. And that, apparently, the brain does this of it's own accord and we are hopeless to predict what exactly will happen.
So comes the disparaging news. The area of this brain that was affected by the bleeding has been damaged, and it won't recover. So he has lost a certain amount of function and only time will tell what he can recover. Since the bleed was on the left side of his brain she suggested that speech and language were likely affected, but how badly and to what end, we don't know.
He's kicking both legs with more or less equal vigour, but his arm is still pretty dead. He will likely always suffer from impairment and weakness in his right limbs, and his arm will probably be worse off than the leg. He'll be getting assessed by a physiotherapist soon, who will determine what we can do to aid him in recovering what function he can, and since we were already on the fast track to getting Ford into several long-term, community-based therapy/development programs, this will likely just get lumped in with the rest of his treatments when we bring him home again.
There has been some disagreement (mostly between Christa and I) about whether what happened to Ford was 'technically' a stroke or not. We hadn't really got a clear answer until today, when the neurologist explained that it was 'technically' a venous stroke, which is mechanically different from the more common arterial strokes, but creates similar types of damage. Not that it really matters, in the end, this bickering over words. But it does make me feel like less of an alarmist when I go around telling people that my son had a stroke.
From the now seemingly insignificant respiratory front (remember when we were so desperately concerned with Ford's breathing and chronic lung collapse?), Ford was extubated to Bipap today, even though he hates it so much it turns him into a writhing, psychotic monkey (or maybe that was the stroke this time). His cry is pretty weak, almost inaudible, but that should hopefully recover over time. He's been hacking up wet, blood streaked phlegm all day, which makes us wonder whether he's come down with tuberculosis too (hey, at this point why not?), but is really just post-intubation irritation. Hopefully we will be back up on the ward by the weekend and if that all goes smoothly we might be home sooner rather than later. Neurology isn't interested in following him very closely anymore, they say it's up to the occupational and physiotherapists, as well as general pediatrics, to decide when he next gets the boot.
She confirmed the relative good news that while nothing had gotten any better, things hadn't gotten worse.
The treatment for his venous sinus thrombosis (brain vein clots), was downgraded from Heparin to Enoxaparin, which is easier on his system long-term, and poses a lower risk of starting new bleeds. The existing clots will take months to break down, if they do at all. She said that only 60-70% tend to fully dissolve and that if they don't the blood will form/find new ways to get out of his head. This happened with Ford's first clot (in his left femoral vein, back in Edmonton), where the blockage has remained but his body has grown multiple collateral connections around it to keep the blood supply moving. This has also happened throughout his chest, prompted by lower than normal oxygen saturation, where (according to his surgeon) a surprising number of collateral pathways had grown into his lungs with the hopes of boosting their blood supply. So from this point of view, Neurology is only interested in seeing Ford in about 3 months time (assuming the seizures don't come back) to do a repeat CT scan and see if there has been any progress in breaking things down.
We were, of course, mostly concerned with how damaging this has been for him and how much loss of function we should expect. Unfortunately it's pretty grey and she was reluctant to give us any definitive answers. But, similar to his circulatory system, if parts of the brain get damaged new pathways are developed. She emphasized the plasticity of infant brains, suggesting that his brain will likely prioritize its functions and make sure that things which are high-priority (like speech and language) get moved to less damaged areas, but that this comes at the price of loosing other abilities that would otherwise occupy those regions. And that, apparently, the brain does this of it's own accord and we are hopeless to predict what exactly will happen.
So comes the disparaging news. The area of this brain that was affected by the bleeding has been damaged, and it won't recover. So he has lost a certain amount of function and only time will tell what he can recover. Since the bleed was on the left side of his brain she suggested that speech and language were likely affected, but how badly and to what end, we don't know.
He's kicking both legs with more or less equal vigour, but his arm is still pretty dead. He will likely always suffer from impairment and weakness in his right limbs, and his arm will probably be worse off than the leg. He'll be getting assessed by a physiotherapist soon, who will determine what we can do to aid him in recovering what function he can, and since we were already on the fast track to getting Ford into several long-term, community-based therapy/development programs, this will likely just get lumped in with the rest of his treatments when we bring him home again.
There has been some disagreement (mostly between Christa and I) about whether what happened to Ford was 'technically' a stroke or not. We hadn't really got a clear answer until today, when the neurologist explained that it was 'technically' a venous stroke, which is mechanically different from the more common arterial strokes, but creates similar types of damage. Not that it really matters, in the end, this bickering over words. But it does make me feel like less of an alarmist when I go around telling people that my son had a stroke.
From the now seemingly insignificant respiratory front (remember when we were so desperately concerned with Ford's breathing and chronic lung collapse?), Ford was extubated to Bipap today, even though he hates it so much it turns him into a writhing, psychotic monkey (or maybe that was the stroke this time). His cry is pretty weak, almost inaudible, but that should hopefully recover over time. He's been hacking up wet, blood streaked phlegm all day, which makes us wonder whether he's come down with tuberculosis too (hey, at this point why not?), but is really just post-intubation irritation. Hopefully we will be back up on the ward by the weekend and if that all goes smoothly we might be home sooner rather than later. Neurology isn't interested in following him very closely anymore, they say it's up to the occupational and physiotherapists, as well as general pediatrics, to decide when he next gets the boot.
Monday, November 9, 2009
another day
Ford had his MRI today, and a picc line put in his right arm. they plan to extubate tomorrow morning. it will be great to hear his voice again.
he didn't come back from all of that business until 4:30pm - too late to get to talk to neurology about any findings, which we figured may happen. we did hear that it looked the same as his last CT scan. which at least tells us it hasn't gotten worse.
they stopped the heparin infusion and have resumed enoxaparin.
no change in the movement of his limbs.
he didn't come back from all of that business until 4:30pm - too late to get to talk to neurology about any findings, which we figured may happen. we did hear that it looked the same as his last CT scan. which at least tells us it hasn't gotten worse.
they stopped the heparin infusion and have resumed enoxaparin.
no change in the movement of his limbs.
Sunday, November 8, 2009
Not much more
He's still sedated and intubated in lieu of tomorrow's MRI/picc line insertion.
There were several moments today where he was relatively alert, looking around, making eye contact. But in general he's still pretty dopey.
His right leg is moving a lot more than yesterday, but is still not as strong as his left leg.
There were times when, being particularly irritated (doing the really uncomfortable silent-screaming-thing that intubated babies do), while wildly flailing and kicking his other limbs, his right arm would move as well. He still won't grab anything that's put into his right hand, and only seems to be able to make uncoordinated jerking motions with the arm. Hopefully it will just take more time.
There were several moments today where he was relatively alert, looking around, making eye contact. But in general he's still pretty dopey.
His right leg is moving a lot more than yesterday, but is still not as strong as his left leg.
There were times when, being particularly irritated (doing the really uncomfortable silent-screaming-thing that intubated babies do), while wildly flailing and kicking his other limbs, his right arm would move as well. He still won't grab anything that's put into his right hand, and only seems to be able to make uncoordinated jerking motions with the arm. Hopefully it will just take more time.
Saturday, November 7, 2009
not much
not many changes today, in Ford or his treatment.
his right leg was moving more today, which is very encouraging, though his right arm remains motionless.
he opened his eyes for a few minutes this afternoon which was also great to see, and both Nick and I took turns holding him in the rocking chair. it reminds me of the early weeks, when it took 3 people to move him into our laps, the delicate transfer of him while intubated.
yes they decided to keep him intubated until tuesday. on monday, he's getting an MRI and a picc line put in, which he'd have to be intubated for anyway. so it's better not to extubate just for one day.
which means they're keeping him pretty sedated, so that he's not too uncomfortable with the tube down his throat. they have discontinued the midazolam and are just running a morphine infusion, and giving occasional chloral.
so we're waiting to get to tuesday. wait wait waiting.
his right leg was moving more today, which is very encouraging, though his right arm remains motionless.
he opened his eyes for a few minutes this afternoon which was also great to see, and both Nick and I took turns holding him in the rocking chair. it reminds me of the early weeks, when it took 3 people to move him into our laps, the delicate transfer of him while intubated.
yes they decided to keep him intubated until tuesday. on monday, he's getting an MRI and a picc line put in, which he'd have to be intubated for anyway. so it's better not to extubate just for one day.
which means they're keeping him pretty sedated, so that he's not too uncomfortable with the tube down his throat. they have discontinued the midazolam and are just running a morphine infusion, and giving occasional chloral.
so we're waiting to get to tuesday. wait wait waiting.
Friday, November 6, 2009
Figurative Heart Failure

Not a whole lot changed today with Ford's condition. He remains pretty dopey, hardly opened his eyes more than a crack today, and wasn't really coherent when he did. He was, however, getting a lot more feisty with his grabbing at the breathing tube and his kicking. Problem is that at the moment he is only able to move his left arm and leg, his right side (which was the side that was seizing, the bleeding being primarily on the left side of his brain) is seemingly paralyzed. While this is likely not going to be permanent, and it is still far to early on in his recovery to predict any outcomes in terms of his potential "loss of function," it is so uncomfortable to watch him wiggle only half his body.
Neurology has so far been strangely absent from his bedside, despite ICU's constant referral (deferral?) to their authority on the matter of fully assessing Ford's situation. Two of them came by today, poked at his right arm and leg, asked about whether or not he had moved them post-stroke, and then left without offering us anything.
A repeat ultrasound of his head showed that so far the bleeding hasn't spread, and might even look a little better, and that otherwise things are the same.
He is being kept on a long-term anti-seizure medication, phenobarbitol, along with infusions of midazolam and morphine, hopefully short-term.
They are weaning the ventilator with the plan of extubating him early tomorrow.
Ford's primary pediatrician, the one who was following him post-discharge, came by today to offer her condolences and get brought up to speed on his condition. She suggested that we take any predictions on his long-term function with a large dose of skepticism, offering that kids who suffer brain injuries often show remarkable resilience to the insult, sometimes making full recoveries when the initial prognosis is grim. There are small signs that things might not end up being as bad as they look to us right now, but like I said, it's still far to early to know anything much at all. And while things certainly aren't peachy, she did also say that she would rather this have happened to him than an episode of heart failure. Her experience suggests that this will be easier for him to get over than any more trouble with his heart. So we take small measures of reassurance and try our best to ignore the depressing stares that everyone is throwing our way.
Yesterday I suffered my own episode of (figurative) heart failure when one of the clinical nursing specialists' eyes filled with tears as she asked if we would mind if she started praying for Ford. No, of course not... but do you have any idea how scary it is to infer from a medical professional that it's become a time for prayer? Having no faith in any benevolent divinity myself, it amounts to throwing in the towel. I'm pretty reliant on the available technologies and Ford's dynamic biology to pull him through this. I do not want to hear about doctors and nurses abandoning their practice for prayer until we're all clear that he's on death's doorstep.
Amen.
Thursday, November 5, 2009
Updates on the Brain Drain
So Ford definitely has a large clot in one of the major veins in his head (can't remember the name of it at the moment, running on 2 days of almost no sleep). Along with the clot there is evidence of bleeding in his brain around the vein, but we're not yet sure how extensive this is. We haven't yet got a detailed report from neurology regarding the CT scan earlier today, and we are anxiously waiting for news of how serious this event was. Cardiology came by to let us know that from their perspective (they looked at his heart circulation during the CT as well) everything is basically as they expect it to be, that the concern of another clot in his superior vena cava was a false alarm. phew, i guess.
Rounds this morning were amazing. They tried to keep us out but Christa very curtly told them to F-off and let us in (although not in so many words). I've never seen so many people around his bed.. in fact there were so many that they filled most of the room, a room with like 8 patient beds in it. And all these doctors were shouting over each other and calling out suggestions and pushing up to try and see him, while x ray carts, and IV trolleys, and Echo machines where being wheeled in and out. It was all a bit overwhelming.
So the trick now is to treat the clot without aggravating the bleeding, but the only treatment for clots are anti-coagulants, which are known to cause bleeding. Hematology spent a good 10 minutes repeating to us that this approach was "a really fine balance" (literally, they just kept saying that over and over again.. very annoying). The danger being that if the clot gets any bigger it could trigger extensive brain damage, but if in treating the clot they prompt the bleeding to spread there will also be extensive brain damage... So we are hoping that this balance can be achieved and maintained, while feeling the acute pressure of being caught between a rock and a hard place.
At the moment Ford is totally stoned. He was bombarded with sedatives this morning to counter the seizures, and has had continuous doses throughout the day to keep him comfortable through all the tests. But now they want to know if he will wake up and show signs of neurological impairment, and he won't because he's been so aggressively beaten up with drugs. There were glimmers of life earlier when he tried half heartedly to pull out his breathing tube (prompting more sedation), and we are told to be reassured by his level of awareness during the seizures (he didn't lose consciousness and was able to track movement with his eyes and grab with his left hand while his right side was trembling). So perhaps for the moment he is still mostly there, but the next few days will be pretty critical in terms of watching how the clot respond to the drugs and keeping the bleeding contained. He is back in fragile condition and we are feeling a stunning bewilderment in the face of how quickly things went wrong.
Walking around the hospital was so utterly jarring today. We've gotten to know so many people here, and their usually friendly faces were all so grim and compassionate. I've never had my shoulder touched so many times in so few hours.. I hope I don't catch swine flu.
Rounds this morning were amazing. They tried to keep us out but Christa very curtly told them to F-off and let us in (although not in so many words). I've never seen so many people around his bed.. in fact there were so many that they filled most of the room, a room with like 8 patient beds in it. And all these doctors were shouting over each other and calling out suggestions and pushing up to try and see him, while x ray carts, and IV trolleys, and Echo machines where being wheeled in and out. It was all a bit overwhelming.
So the trick now is to treat the clot without aggravating the bleeding, but the only treatment for clots are anti-coagulants, which are known to cause bleeding. Hematology spent a good 10 minutes repeating to us that this approach was "a really fine balance" (literally, they just kept saying that over and over again.. very annoying). The danger being that if the clot gets any bigger it could trigger extensive brain damage, but if in treating the clot they prompt the bleeding to spread there will also be extensive brain damage... So we are hoping that this balance can be achieved and maintained, while feeling the acute pressure of being caught between a rock and a hard place.
At the moment Ford is totally stoned. He was bombarded with sedatives this morning to counter the seizures, and has had continuous doses throughout the day to keep him comfortable through all the tests. But now they want to know if he will wake up and show signs of neurological impairment, and he won't because he's been so aggressively beaten up with drugs. There were glimmers of life earlier when he tried half heartedly to pull out his breathing tube (prompting more sedation), and we are told to be reassured by his level of awareness during the seizures (he didn't lose consciousness and was able to track movement with his eyes and grab with his left hand while his right side was trembling). So perhaps for the moment he is still mostly there, but the next few days will be pretty critical in terms of watching how the clot respond to the drugs and keeping the bleeding contained. He is back in fragile condition and we are feeling a stunning bewilderment in the face of how quickly things went wrong.
Walking around the hospital was so utterly jarring today. We've gotten to know so many people here, and their usually friendly faces were all so grim and compassionate. I've never had my shoulder touched so many times in so few hours.. I hope I don't catch swine flu.
Seizures! Yay!
Ford started having seizures at 2am this morning, prompting an overwhelming flood of people into our room to administer heavy doses of sedatives and paralytics. The seizures lasted for about 2 hours until the aforementioned intervention brought them under control. Because he was so heavily knocked out they had to intubate him, so we are back in the ICU. Tuesday's voluntary trip back to the hospital with only a mild concern about a loose suture has been spinning out of control over the last 48 hours (beginning with Ford going back on oxygen support yesterday because a blood test showed his hemoglobin was unexpectedly high - which, if left to rise too high turns your blood into a thick sludge - Ford's bone marrow is trying to compensate for his low oxygen saturation by producing higher levels of hemoglobin, which carry oxygen through the blood). So much for our two day stay. By 5am they had Ford stabilized on the ventilator, were busy with the now routine comedy of attempts at getting a working IV in him, and by 6 he was being wheeled into radiology for a CT scan of his brain to try and figure out what the problem might be.
It's worth pointing out that Dr. Human had scheduled a CT scan on Ford's head for today anyway, just as a precaution, to rule out anything going on upstairs that might explain his persistant irritability. It's not unusual for kids who've had the 'Glen' surgery to experience intense head-aches from the higher pressures in their veins. And apparently a potential side effect of the anti-coagulant treatment that Ford has been getting for months now is bleeding in the brain, so that is also something they were hoping to 'not see.' Despite being a bit frightened by the prospect of something like that going wrong we were reassured by the Laurie, the CNS, that everything would likely be fine as Ford was not exhibiting any clinical signs of brain trauma - aka, seizures.
So. Now he is.
Just got an update from the intensivist while I was writing this that they did see some bleeding on the left side of his brain under the CT scan but that they weren't sure yet what was causing it. Neurology, Neurosurgery, Cardiology, and Hematology are all apparently clustered around the computer watching the pictures and trying to sort it out. So, suspicions are potentially being confirmed here that it is a small bleed (or subarachnoid hemorrhage) as a result of him being overly anti-coagulated, but it might also be a venous sinus thrombosis, which is the result of having too little anti-coagulant (compounded perhaps by Ford's thick, hemoglobin heavy blood). From what i gathered, the bleeding isn't too bad and they aren't thinking of a surgical intervention at this point. They're just going to let him wake up and then wait and watch.
Rounds sure will be interesting today. If the ICU staff lets us in.
We sure enjoyed our two week holiday from the hospital.
It's worth pointing out that Dr. Human had scheduled a CT scan on Ford's head for today anyway, just as a precaution, to rule out anything going on upstairs that might explain his persistant irritability. It's not unusual for kids who've had the 'Glen' surgery to experience intense head-aches from the higher pressures in their veins. And apparently a potential side effect of the anti-coagulant treatment that Ford has been getting for months now is bleeding in the brain, so that is also something they were hoping to 'not see.' Despite being a bit frightened by the prospect of something like that going wrong we were reassured by the Laurie, the CNS, that everything would likely be fine as Ford was not exhibiting any clinical signs of brain trauma - aka, seizures.
So. Now he is.
Just got an update from the intensivist while I was writing this that they did see some bleeding on the left side of his brain under the CT scan but that they weren't sure yet what was causing it. Neurology, Neurosurgery, Cardiology, and Hematology are all apparently clustered around the computer watching the pictures and trying to sort it out. So, suspicions are potentially being confirmed here that it is a small bleed (or subarachnoid hemorrhage) as a result of him being overly anti-coagulated, but it might also be a venous sinus thrombosis, which is the result of having too little anti-coagulant (compounded perhaps by Ford's thick, hemoglobin heavy blood). From what i gathered, the bleeding isn't too bad and they aren't thinking of a surgical intervention at this point. They're just going to let him wake up and then wait and watch.
Rounds sure will be interesting today. If the ICU staff lets us in.
We sure enjoyed our two week holiday from the hospital.
Wednesday, November 4, 2009
oh bother
Ford is back in the hospital, though not for what we worry most about - respiratory distress or heart failure - but potential infection. the incision on his chest bled a bit monday night and by tuesday morning stiches had poked themselves out of the skin and the area was red and puffy.
dr. Human thought sending him home on oral antibiotics would be a safe course, but after surgeon dr. Campbell took a look at it he admitted Ford and ordered IV antibiotics - they act faster.
in the meantime, while looking at his incision, we also talked about Ford's high level of irritability. we've been attributing some of it to his frequent vomiting/gagging fits - which haven't increased in frequency of late (10-15 times a day) but each "attack" has been lasting longer, up to 10 awful minutes each time. instead, dr. Human pondered it could be very bad post-Glenn headaches that are keeping Ford unhappy (note he isn't entirely unhappy - but since the Glenn he has not been the same baby as he was before). headaches are caused by the increase pressure in the head, now that the SVC is moving blood simply by gravity, instead of being pumped by the heart. these headaches can last a couple post-op months at least, but dr. Human wants to rule out anything worse than just increased pressure - like a missed clot. they've ordered a CT scan of Ford's brain. that test will take place tomorrow.
speaking of clots, the one formed in Ford's left ventricle has come down in size and they discontinued Ford's twice daily enoxaparin injections. hurrah! no more stabbing needles into his thighs. we're pleased with that. Ford will be kept on some aspirin instead.
the feeding study Ford had last week went perfectly - he swallows well, with a good rhythm, and he protects his airway when swallowing or crying. so that was assuring. it does mean that his vomiting thing is therefore not caused by an uncoordinated swallow.
they haven't seen an HLHS baby with this gagging problem before and their lack of insight is disheartening.
as you can guess, being back in the hospital is also disheartening, though very familiar. the treatment is done over the course of 48 hours, so hopefully the stay isn't any longer than that.
dr. Human thought sending him home on oral antibiotics would be a safe course, but after surgeon dr. Campbell took a look at it he admitted Ford and ordered IV antibiotics - they act faster.
in the meantime, while looking at his incision, we also talked about Ford's high level of irritability. we've been attributing some of it to his frequent vomiting/gagging fits - which haven't increased in frequency of late (10-15 times a day) but each "attack" has been lasting longer, up to 10 awful minutes each time. instead, dr. Human pondered it could be very bad post-Glenn headaches that are keeping Ford unhappy (note he isn't entirely unhappy - but since the Glenn he has not been the same baby as he was before). headaches are caused by the increase pressure in the head, now that the SVC is moving blood simply by gravity, instead of being pumped by the heart. these headaches can last a couple post-op months at least, but dr. Human wants to rule out anything worse than just increased pressure - like a missed clot. they've ordered a CT scan of Ford's brain. that test will take place tomorrow.
speaking of clots, the one formed in Ford's left ventricle has come down in size and they discontinued Ford's twice daily enoxaparin injections. hurrah! no more stabbing needles into his thighs. we're pleased with that. Ford will be kept on some aspirin instead.
the feeding study Ford had last week went perfectly - he swallows well, with a good rhythm, and he protects his airway when swallowing or crying. so that was assuring. it does mean that his vomiting thing is therefore not caused by an uncoordinated swallow.
they haven't seen an HLHS baby with this gagging problem before and their lack of insight is disheartening.
as you can guess, being back in the hospital is also disheartening, though very familiar. the treatment is done over the course of 48 hours, so hopefully the stay isn't any longer than that.
Sunday, November 1, 2009
a walk in the park
Subscribe to:
Posts (Atom)










